What you should know:
– Oussourthe leader in AI-powered customer experience automation (CXA), announced the launch of pre-built, self-service solutions designed to revolutionize care navigation for health plans and third-party administrators (TPAs).
– THE Powered by AI The tools address the growing need for effective and efficient support for members, particularly to help them navigate complex health journeys such as pregnancy and chronic illness.
Addressing the challenges of navigating care
Today’s health care landscape presents significant challenges for health plans and health plan administrators. The current system often relies on limited human resources, making it difficult to proactively support members with complex care needs. This reactive approach is particularly problematic for chronic and mental illness, which account for 90% of the country’s $4.1 trillion in annual health care spending, according to the CDC.
Ushur’s AI Approach
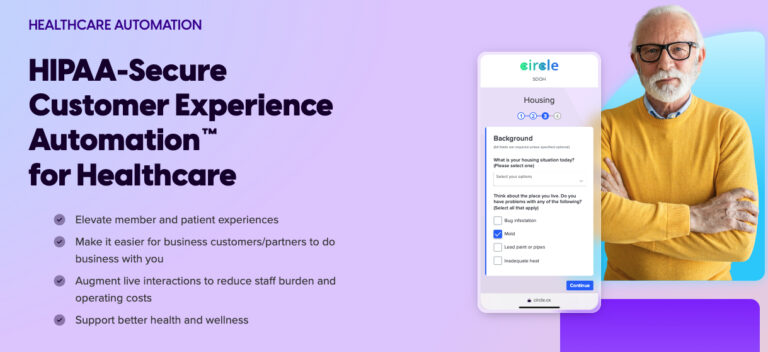
Ushur addresses these challenges with its AI-powered solutions. These tools focus on identifying and automating key communication points throughout critical care pathways. Delivered through secure, interactive, and HIPAA-compliant digital experiences, Ushur’s solutions aim to:
- Improving health outcomes: Motivate positive behavior changes and prevent costly complications associated with disengaged patients.
- Simplify processes: Automate tasks and processes, freeing up live resources for more complex interactions.
- Improve member engagement: Proactively guide members and provide relevant resources at critical touchpoints.
Pre-built solutions for common care pathways
Ushur offers two pre-defined solutions tailored to members’ specific needs:
- Navigating Maternal and Newborn Health Care: Guides expectant mothers and new parents through prenatal and postpartum care, promoting better health outcomes for mother and child.
- Navigating Care for Chronic Diseases: Enables members with chronic conditions, such as diabetes or musculoskeletal issues, to connect with the right resources and adopt healthier habits, ultimately leading to better health and reduced costs.
Field-tested solutions produce measurable results
Ushur’s pre-built solutions are powered by industry-leading AI and automation, pre-tested by the nation’s leading health plans. These tools address key areas to streamline care navigation and member support:
- Education: Proactive guidance and provision of resources at critical points in a member’s care journey.
- Sensitization : Regular communication and personalized care plans based on member feedback.
- Coordination: Assistance in scheduling appointments with specialists and identifying resources outside the health insurance plan network.
- Management: Automated document processing and data upload to back-end systems, eliminating manual intervention.
Designed for efficiency, security and scalability
Ushur’s CXA platform prioritizes speed to value, enterprise-grade security, and operational efficiency. The platform enables effective care management through bi-directional, digital interactions via HIPAA-secure and HITRUST-certified channels.
“The U.S. healthcare system remains incredibly challenging. Both payers and members pay significantly higher costs when appropriate care and resources are not understood and utilized in a timely manner, particularly in complex care situations,” said Yvonne Daugherty, global industry leader at Ushur. “The National Institute of Health (NIH) estimates that failures in care coordination account for nearly $80 billion in costs annually. Ushur launched these care navigation automation solutions to help dramatically improve the member experience while achieving significant cost savings not only for healthcare payers but for the nation’s entire healthcare system. Our vision is to continue to alleviate pressure on an overburdened national healthcare system while enabling payers and providers to deliver transformative experiences to their members, particularly those in critical health situations.”